Hip painBe specific An unpleasant, unbearable sensation caused by pathology of the upper femur, acetabulum, and nearby soft tissue structures. In terms of strength, they range from weak to unbearable, and in nature they can be blunt, sharp, oppressive, painful, bursting, drilled, etc. They usually depend on load, time of day, and other factors. The cause of pain is determined by X-ray, CT, MRI, ultrasound, arthroscopy and other studies. Before making a diagnosis, it is recommended to use painkillers and limb rest.
An unpleasant, unbearable sensation caused by pathology of the upper femur, acetabulum, and nearby soft tissue structures. In terms of strength, they range from weak to unbearable, and in nature they can be blunt, sharp, oppressive, painful, bursting, drilled, etc. They usually depend on load, time of day, and other factors. The cause of pain is determined by X-ray, CT, MRI, ultrasound, arthroscopy and other studies. Before making a diagnosis, it is recommended to use painkillers and limb rest.
Causes of hip pain
Soft tissue injury
The most common cause of traumatic pain is hip contusion. It occurs when falling on the side or directly hitting it, manifests as moderate acute pain, quickly becomes dull, gradually decreases and disappears within a few days, in severe cases-several weeks. The support is retained and the movement is slightly restricted. Edema is locally detected and bruising may occur.
Hip ligament injuries are rare, usually the result of road traffic accidents and sports injuries, accompanied by severe pain, and sometimes-a feeling of cracking (such as tearing tissue). The pain is reduced, and then often worsened by edema. The swelling extends from the joints to the groin area, thighs.
The degree of dysfunction of ligament organ trauma depends on the severity of the injury (stretched, torn, ruptured), ranging from slightly restricted to unable to support the leg. The pain increases with the deviation of the trunk, and the direction of movement is opposite to the damaged ligament.
Bone and joint injuries
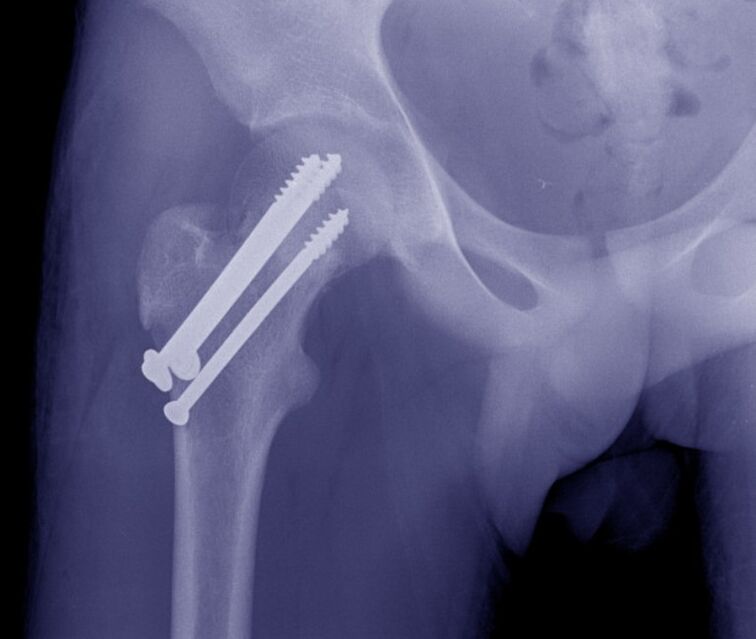
Due to family or street trauma, hip fractures usually occur in the elderly. One characteristic, especially in the presence of osteoporosis, is the absence of severe pain syndrome and mild edema. At rest, the pain is deep, dull, moderate or insignificant. With exercise, the pain sensation increases sharply. Sometimes support is retained. A common symptom is the inability to lift the straight leg from the prone position (a symptom of a stuck heel).
Intertrochanteric fractures are more common in middle-aged and young people and are the result of high-energy trauma. Unlike cervical spine fractures, they are accompanied by severe, diffuse deep pain that is unbearable. Then the pain eased, but it was still very strong and unbearable. The joints are swollen and may be bruised. Movement is severely restricted. Support is impossible.
Isolated fractures of the greater trochanter are rare; they are seen in children and young adults; they are formed by falls, direct impacts, or sharp muscle contractions. The pain is severe, very intense, and is mainly located on the outer surface of the joint. Due to the increased pain, the patient avoids active exercise.
Hip dislocation occurs during falls from heights, industrial and road traffic injuries, and manifests as unbearable severe pain that will hardly be relieved until relief. Deformation of the joints, shortening of the legs, bending of the knee joint, turning outwards, and turning inwards less (depending on the type of dislocation). Support and movement are impossible. When trying to move, the spring resistance is determined.
Acetabular fractures occur alone or combined with hip dislocation. It is characterized by acute burst pain deep in the hip joint. Subsequently, the pain was reduced, but still strong, hindering any movement. The legs are shortened and rotated outward. Support is impossible.
Degradation process
In the early stage of hip joint disease, the pain is periodic, dull, and unclear. It appears at the end of the day or after a significant load, and sometimes radiates to the hip and knee joints. A slight, fast-passing stiffness may appear at the beginning of the exercise. Subsequently, the intensity of pain increases, not only during exercise, but also during rest. After strenuous exercise, the patient began to limp. Movement is somewhat restricted.
In severe hip joint disease, the pain is deep, diffuse, continuous, painful, and distorted. Both day and night. The resistance to pressure is reduced; the patient is leaning on crutches when walking. Obviously restricted movement, shortened limbs, increased joint load, and increased pain during walking and standing.
The course of hip chondroma is similar to subacute arthritis. The pain is moderate, diffuse, and short-lived, with crunching noises and limited mobility. When the intra-articular body is invaded, blockage occurs, which is characterized by severe pain, inability or obvious limitation of movement. After the end of the infestation of joint mice, the listed symptoms disappeared.
Trochantitis is usually formed by arthropathy of the hip joint, accompanied by inflammatory degenerative lesions of the gluteal muscle tendon at its connection point with the greater trochanter, which is manifested in the painful side of the affected area in the supine position. When trying to abduct the hip joint with resistance, the pain increases.

Osteodystrophy
Perthes disease occurs most frequently in children and adolescents. It is characterized by local necrosis of the femoral head. It is initially accompanied by mild, blunt and deep pain, sometimes radiating to the knee and hip joints. After a few months, the pain intensified sharply, becoming persistent, intense, and exhausted. Swelling of the joints, restricted movement, and limp. Then the pain was relieved and the joint function recovered to varying degrees.
Aseptic necrosis downstream of the femoral head is similar to Perthes disease, but it is detected in adults and progresses less smoothly, and is bilateral in half of the cases. At first, the pain was periodic, pulling. Then the pain syndrome worsens and appears at night. At the peak of clinical manifestations, the pain is so severe that the patient completely loses the ability to lean on his legs. Then the pain gradually reduced. Movement is restricted for about 2 years, and the result is hip joint arthropathy, contractures, and limb shortening.
A 10-15 year old boy’s proximal thigh metaphysis developed a solitary bone cyst with non-severe intermittent pain in the hip joint. Edema is usually absent, and prolonged contractures often occur, especially in young children. As the symptoms are mild, the cause of treatment is a pathological fracture or restriction of movement.
arthritis
Aseptic arthritis manifests as wavy pain in the joints and increases before the morning. The severity of pain ranges from insignificant to severe, intense, continuous, and significantly restricting physical activity. Note stiffness, swelling, redness, and local temperature increase. Palpation is painful.
In rheumatoid arthritis, the hip joint is rarely affected and the lesions are symmetrical. Periodic pain first appears in the context of seasonal changes (autumn, spring), rapid changes in weather conditions, hormonal changes after childbirth, or menopause. The pain is moderate or weak, diffuse, stretched or painful, and aggravates sharply on palpation. It is combined with recurrent synovitis, edema, congestion, and high fever to increase restriction of activity.
Infectious arthritis develops with the blood-borne or lymphatic spread of the infection, and is less common-as the pathogen penetrates into the joints from nearby tissues. The onset is usually acute and the pain worsens rapidly. The pain is severe, convulsions, tears, ruptures, annoying during rest, and aggravated during exercise, so the limb adopts a forced posture. The patient has fever, chills, sweating, severe weakness, edema, redness of the joints, and elevated local temperature.
If not treated in time, bacterial infectious arthritis can become total arthritis-purulent inflammation of all tissues in the hip joint. It is characterized by a severe course of the disease, accompanied by very acute widespread pulsating pain, hot flashes, severe weakness, pre-syncope, obvious congestion and hyperthermia.
Other inflammatory diseases
Osteomyelitis of the upper thigh can be blood-borne, post-traumatic, or postoperative. Hematogenous osteomyelitis is manifested by obvious localized, very severe bursts, convulsions, tears, or boring pain, so the patient avoids the slightest limb movement. There is obvious high fever and serious poisoning.
The occurrence of post-traumatic and postoperative osteomyelitis has similar but less obvious symptoms. Usually, the onset occurs more slowly against the background of open fractures or postoperative wounds, and purulent discharge appears. Hip pain increases as signs of local inflammation progress within 1-2 weeks.
Synovitis develops in the context of injuries and other diseases of the hip joint, and rarely becomes a manifestation of allergies. In acute synovitis, the pain is usually mild, dull, bursting, and gradually worsened due to the increase in the amount of intra-articular fluid. Joint swelling, slight pain on palpation, confirmed fluctuating symptoms. Chronic synovitis is asymptomatic and is accompanied by mild pain.
Intermittent joint effusion, pain is not obvious, accompanied by discomfort, and limited mobility, which disappears within 3-5 days after the reverse absorption of the effusion. They are updated regularly, each patient is different, and are caused by repeated accumulation of fluid in the joints.
Specific infection
Hip tuberculosis is a common form of bone and joint tuberculosis, which manifests as general weakness, fatigue, and fever. Then the muscles are weakly stretched or sore, and there is a short-term pain in the joints when walking. The patient began to retain his limbs. As the pain progresses, they become mild, diffuse, radiate to the knee, and are accompanied by swelling, redness, and synovitis. Development of protective contractures.
Brucellosis may cause joint pain, including hips. In the acute and subacute forms, the pain is pulling and twisting, accompanied by periodic fever, swollen lymph nodes, and skin rashes. In the chronic course, the pain syndrome is similar to aseptic arthritis, which will form deformities over time.
Congenital abnormalities
The performance of hip dysplasia depends on the degree of disharmony between the femoral head and the acetabulum. Complete congenital dislocation, pain immediately after the child starts walking, accompanied by claudication. For moderate subluxation, pain occurs at 5-6 years of age, which is directly related to the load on the legs.
Mild subluxation, pathologically asymptomatic for a long time, pain syndrome manifested as the development of dysplastic hip joint disease in 25-30 years old. This joint disease is characterized by a rapid increase in pain, early onset of rest and night pain, and gradual limitation of movement. All forms of dysplasia are accompanied by asymmetry of skin folds, "click" symptoms and restricted mobility. In the case of dislocation, notice the shortening of the limbs.
Tumor
For benign tumors, a typical asymptomatic course. The pain is mild, intermittent, and usually does not progress over the years. Tumor growth is accompanied by a slow increase in pain syndrome and recurrent synovitis. In the hip joint area, osteoma, osteoid osteoma, osteoblastoma, and chondroma are more commonly detected.
Malignant tumors (osteosarcoma, chondrosarcoma) are characterized by the rapid progression of pain syndromes and other pathological manifestations. At first, the pain is mild, short-term, without a specific location, and sometimes worse at night. Later, they become sharp, permanent, cut, surround, and spread throughout the joint. The affected area is swollen and deformed. Note weight loss, weakness, and low-grade fever. For advanced tumors, only the use of anesthetics can eliminate pain and unbearable pain.
other reasons
Hip joint pain sometimes appears with lumbosacral plexitis and sciatic neuropathy. However, they usually occupy a negligible position in the clinical manifestations of the disease. Compared with the severe pain in the hips and back of the thigh, and the weakness of the limbs, they gradually fade out of the background. And sensitivity barriers.
This localized pain syndrome is usually detected in osteochondrosis and intervertebral disc herniation. Pain can be detected by spondylitis, spondyloarthropathy and curvature of the spine. Pain is dull, cyclical, painful, and usually worsens during the worsening of the underlying disease. The reason for their appearance may be the continuous overload of the joints or the development of hip joint disease.
Sometimes joint pain is caused by mental illness or depression. Diabetes is often accompanied by enthesal disease, bursitis, and other soft tissue lesions around the joints. Drug-induced joint disease may occur when taking certain drugs.
diagnosis
In the case of injury, diagnostic measures are carried out by a traumatologist. Degenerative and inflammatory diseases are managed by orthopedic doctors and rheumatologists. In the case of a suppurative process, the involvement of the surgeon is necessary. Inspection includes collecting complaints, studying medical history, physical examination, and supplementary research. Taking into account the particularity of the pathological process, the following methods can be used:
- Radiography.It is the basic technique for most joint diseases. Detect fractures, dislocations, changes in the contours of the acetabulum and femoral head, margins and intraosseous defects, bone growth, and narrowing of the joint space.
- Ultrasound.The most useful information when studying soft tissues. Reveal signs of inflammation and degenerative processes, calcified areas. Used to diagnose effusion and joint mice.
- MRI and CT.In the case of unclear basic research data, use clarification techniques to clarify the nature, generality and location of the pathological focus. Can be compared.
- Joint puncture.It has diagnostic or therapeutic and diagnostic properties. Allows you to remove fluid accumulation, study the composition of intra-articular fluid, and use laboratory tests to determine the pathogen of the infection.
- Arthroscopy.During the visual inspection of the joints, the doctor will assess the condition of the bones and soft tissue structures, and if necessary, will collect biopsy samples for subsequent histological examinations and take treatment measures.
- lab testing.They are used to determine signs of inflammation and markers of rheumatism to assess the general condition of the body, the activity of various organs in severe infections or systemic pathologies.
treatment
Help before diagnosis
In the case of a serious injury, it is necessary to fix the joint by using a splint from the foot to the armpit. In the case of minor trauma, enough to rest the legs. Apply cold compresses to the affected area. For severe pain, give analgesics. You can't use your limbs for active movement, load your legs. It is strictly forbidden to try to eliminate the dislocation or displacement of bones.
The strategy of non-traumatic disease is determined by symptoms. For minor manifestations, you can ensure that the rest of the limbs are treated with local therapies that have analgesic and anti-inflammatory effects. If fever, weakness, severe pain, rapid growth of edema, congestion, etc. occur, it is recommended to seek professional help immediately.
Conservative treatment
Dislocation is a sign of immediate reduction. In the case of a fracture, bone traction is usually applied, and then after signs of callus appear, the patient is operated on or the limb is fixed with a plaster cast. For elderly patients with hip fractures, it is allowed to use unwinding boots to prevent joint rotation.
It is recommended that the remaining patients relax their hip joints. According to the indications, orthotics or additional devices (crutches, canes) are recommended. Prescribe massage, physiotherapy exercises, physiotherapy procedures:
- Laser Treatment;
- Magnetic therapy;
- UHF
- Ultrasound
- Drug electrophoresis;
- Ultra high temperature and high pressure.
Non-steroidal anti-inflammatory drugs, chondroprotective agents, and antibacterial drugs can be used. Local agents are widely used. According to the indications, joint puncture, intra- and peri-articular blockage with hormones, intra-articular injection of chondroprotective agents, synovial fluid substitutes
surgery
The operation of the hip joint is performed through open surgery with the help of arthroscopic equipment. Considering the type of pathology, you can do the following:
- trauma:Open reduction of hip dislocation, acetabular reconstruction, neck osteosynthesis, trochanter fracture.
- Degradation process:Arthrotomy, arthroscopy, removal of free intraarticular body.
- Tumor:Removal of tumor, bone resection, hip dislocation, Io-abdominal amputation, Io-abdominal resection.
It is performed in the case of contracture, joint ankylosis, scarring of the tissue around the joint, correction, arthroplasty and arthrodesis. Endoprostheses are an effective way to restore limb function in diseases of various origins, accompanied by restricted movement or joint destruction.



































